Budget 2023 must address Healthcare Inequalities
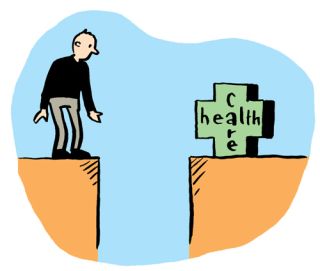
People should be assured of the required treatment and care in times of illness or vulnerability. The standard of care is dependent to a great degree on the resources made available, which in turn are dependent on the expectations of society. Covid-19 put an unprecedented strain on our healthcare system and its workers, with the full cost yet to be reckoned with.
Access to Care
Ireland ranked 22nd out of 35 countries in 2018 in a report by Health Consumer Powerhouse published in 2019, but on the issue of accessibility, Ireland ranked the worst. That report notes that even if the (then) Irish waiting-list target of 18 months were reached, it would still be the worst waiting time situation in Europe. Irish hospitals are working near full capacity.
According to data from the National Treatment Purchase Fund there were 624,444 people waiting for outpatient’s treatment in May 2022, with 138,757 patients (including more than 20,000 children) waiting for 18 months or more for treatment. While the pandemic may have contributed to the numbers on the waiting lists in recent times, the numbers have been very high over many years, and well above 400,000 since 2015. The pandemic also limited access to care for people with health conditions not related to COVID-19 and unmet needs for medical care because of delayed or missed consultations are likely to lead to poorer health outcomes in the future. Government needs to urgently address these inequalities in the health service and implement a programme that provides access on the basis of need.
Transforming Acute and Community Care Services
Irish hospitals are working near full capacity. The occupancy rate for acute care beds is among the highest in OECD countries, and while having a high utilisation rate of hospital beds can be a sign of hospital efficiency, it can also mean that too many patients are treated at the secondary care level. In 2019, bed occupancy rates for curative (acute) care were 95 per cent in Ireland, above the capacity considered safe.
Like the governments of other countries, the Irish government made significant additional allocations in 2020 and 2021 to the health sector to deal with the COVID-19 pandemic. These commitments included expanding hospital capacity, developing primary and community-based responses, procurement of medical equipment, and an assistance scheme for private nursing homes. Universal health coverage is a key pre-requisite to improving access to care for vulnerable groups, something, that might be said to be acknowledged in the government’s extension of coverage for GP visits for COVID-19 treatment to the entire population.
The model of healthcare used in Ireland is defined by an over-emphasis on hospitals and acute rather than primary and social care being more central. Social Justice Ireland welcomed the allocation of €240m in 2022 for the rollout of the 96 Community Healthcare Networks and the 30 Community Specialist Teams for Older People & Chronic Disease. However significant sustained investment in General Practice, Primary Care & Community Based Services is required in conjunction with the implementation of the Regional Health Areas to ensure the transformation of the health service in line with Sláintecare.
Proposals: To address the inequalities in our healthcare system and develop a system that is fit for purpose for all, Government needs to:
- Invest €100m in the further expansion of the Enhanced Community Care Programme to alleviate pressure on acute services and ensure treatment is provided at the appropriate level of need.
- Invest the €500m infrastructure allocation set out in Sláintecare with a particular focus on Enhanced Community Care.
- Invest a minimum of €100m annual in providing Universal Access to GP Care while expanding the number of GP and Practice Teams in line with the shift towards Primary Care & Community Based services envisaged in Sláintecare.
- Invest €50m in Community Nursing Facilities and rehabilitation beds.
Mental Health
According to the latest available data, the HSE Management Data Report for March 2021, 2,625 children and young people were awaiting supports from the Child and Adolescent Mental Health Service (CAMHS), with over one in ten waiting for 12 months of more. A mental health crisis is also likely to be a prevailing legacy from Covid-19.
Proposal: Invest in the full implementation of the Sharing the Vision policy (including addressing staffing issues) at a cost of €35m and increase funding for programmes dealing with alcoholism and addictions at a cost of €76m.
Persons with a Disability and Carers
People with disabilities were cumulatively affected by a range of decisions introduced as part of successive austerity Budgets. These included cuts to social welfare payments, changes in medical card eligibility, increased prescription charges, and cuts to supports such as respite, home support hours, and housing adaptation grants. The cumulative effect of changes makes it difficult for some people to continue to live in their communities.
Proposal: To support people with disabilities to live fulfilling lives within their communities, Government must:
- Introduce a cost of disability payment of €20 per week at a cost of €246m in Budget 2023.
- Increase investment in disability services, including respite and personal assistant services (cost of €40m).
- Allocate €40m for implementation of the UNCRPD.
Proposal: To acknowledge and support the work of carers in Ireland, at the very minimum in Budget 2023 Government must:
- Increase the Domiciliary Care Allowance to €330 at a cost of €11.4m.
- Expand the Free Travel scheme to include people in receipt of Domiciliary Care Allowance (cost of €6.1m).
- Increase the annual Carer's Support Grant to €2,000 (at a cost of €21.5m).
- Implement an independent review of Carer’s Allowance.
Budget Choices 2023 is available to download now.