Healthcare inequalities persist and undermine treatment and care
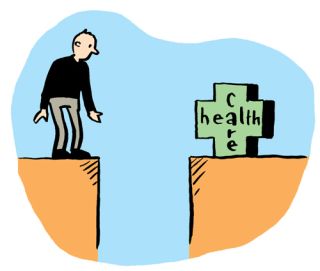
People should be assured of the treatment and care they need in their times of illness or vulnerability. However, the pandemic has shown that Ireland’s healthcare system fails to deliver that treatment and care on the scale required. While our health system, and its workers, have been placed under tremendous pressure due to the COVID-19 pandemic since March 2020, one of the most obvious concerns about the Irish Healthcare system is to do with access. Ireland’s complex two-tier healthcare system means that private patients have speedier access to both diagnostics and treatment, while those in the public system can spend lengthy periods waiting for a first appointment with a specialist and for treatment.
Social Justice Ireland's Policy Briefing, 'Healthcare in Ireland', published today concludes that even though Ireland spends more per capita on health than the EU average, the number of beds per 1,000 population is considerably less than the EU average. Furthermore, a mental health crisis is likely to be a prevailing legacy from Covid-19, not just because of the immediate stress, but also because the impact of the illness on those who contract it and their wider circle. There are similar impacts on healthcare workers and other frontline staff, and on those who live in vulnerable households, including households with domestic abuse
Main findings of Report
- The current global public health crisis is unprecedented and has been termed the worst in a century. Ireland remains the only western European country without universal coverage for primary care.
- Covid-19 has exacerbated many issues in society, not least when it comes to healthcare. According to data from the National Treatment Purchase Fund there were 178,064 people waiting for 18 months or more for outpatient’s treatment in March 2021. This equates to almost three in every 10 of the 628,756 people awaiting treatment that month.
- One of the most obvious concerns about the Irish Healthcare system is to do with access. Ireland’s health system ranked 22nd out of 35 countries in 2018, but on the issue of accessibility, Ireland ranked worst.
- According to the latest available data 2,112 children and young people were awaiting supports from the Child and Adolescent Mental Health Service (CAMHS). Of these one in ten were waiting for treatment for 12 months or more. This is a slight proportionate decrease on the same period in 2019 when 11 per cent were waiting in excess of 12 months or more, and on September 2018 when the proportion was 13 per cent.
- Before the onset of COVID-19 the Irish public hospital system was already operating under pressure from high population growth and ageing, and because of system cuts to bed capacity in the preceding decade.
Certain groups continue to experience health difficulties and need a particular policy focus, and inequalities still need to be addressed as disparities, such as in life-expectancy, continue to be great between socioeconomic groups.
Policy Priorities for consideration
- Ensure that announced budgetary allocations are valid, realistic and transparent and that they take existing commitments into account.
- Complete the roll-out of the Community Health Networks across the country and thus increase the availability and quality of Primary Care and Social Care services.
- Ensure medical card-coverage for all people who are vulnerable.
- Act effectively to end the current hospital waiting list crisis.
- Create a statutory entitlement to Home Care Services. This will require increased funding, but will save the State money long-term, as home support allows people to remain living in their own homes, rather than entering residential nursing care.
- Properly resource and develop mental health services, and facilitate campaigns giving greater attention to the issue of suicide.
- Work towards full universal healthcare for all. Ensure new system structures are fit for purpose and publish detailed evidence of how new decisions taken will meet healthcare goals.
- Enhance the process of planning and investment so that the healthcare system can cope with the increase and diversity in population and the ageing of the population projected for the next few decades.
- Ensure that structural and systematic reform of the health system reflects key principles aimed at achieving high performance, person-centred quality of care and value for money in the health service.
Ireland must decide what services are required, how these should be funded and prioritized (geographically and in other respects). Obtaining value for money is essential, but efficiencies must be delivered without compromising the quality of the service and without disproportionately disadvantaging poorer people. As well as a debate on the overall budget for healthcare, there should be transparency on the allocation to each of the services. Reform will require investment before savings can be made.