Social Prescribing
Our thinking on wellness and staying healthy is expanding. Social prescribing acknowledges that our health and wellbeing can be impacted by social factors such as poverty, local environment, poor housing, isolation and loneliness and offers health professionals a means of referring people to a wide variety range of non-clinical community supports which can have significant benefits for their overall health and wellbeing.
A new Report from the National Academy for Social Prescribing, 'Social Prescribing Around the World', sets out 'Global Developments in Social Prescribing Across Different Health System Contexts'.
Global Focus
The aim of the Report was to explore social prescribing developments across 24 countries. They note that there was no 'single best model or practice of social prescribing'. As health systems will differ across the world, the extent, type and level of social prescribing needs to adapt accordingly. They present 24 case studies of social prescribing which demonstrate that adaptability, setting out the differences and the similarities in approach and practice.
Social prescribing policies make more and more sense in a world with ageing populations and longer life expectancies. We are living longer but that means that more of us will experience disease in old age for a longer period of time. The Report notes that " reactionary and fragmented sick-care health system models designed to only mitigate disease symptoms are insufficient" and we must address the " urgent need to make future health systems and service use more sustainable".
Benefits of Social Prescribing
The organisations and services that people are referred to as part of social prescribing are varied and broad. They will also depend on the person and the options that are available locally. These can include anything from physical activity initiatives like Parkrun and other types of walking groups to reading groups, adult education and other library services as well as men’s and women's sheds, gardening and craft activities.
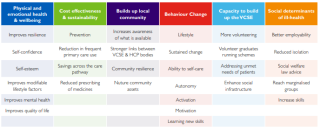
In 2016, the Social Prescribing Network asked social prescribing stakeholders to list the outcomes achieved by social prescribing (See Fig 1).
Figure 1: Outcomes described from social prescribing stakeholders
Social Prescribing in Ireland
The Report tracks the development of Social Prescribing in Ireland and notes that "Social prescribing has significant policy mandate in Ireland and .....started in Ireland as a ground up movement in partnership between the health service and community voluntary sector. Social prescribing services are now available in over 30 locations, including acute hospital settings". Programme for Government : Our Shared Future commits to expanding "social prescribing where patients are referred to non-clinical activities, as a means of positively influencing mental wellbeing" and Sharing the Vision: A Mental Health Policy for Everyone states that "Social prescribing should be promoted nationally as an effective means of linking those with mental health difficulties to community-based supports and interventions, including those available through local Voluntary and Community Sector supports and services".
The Sláintecare Implementation Strategy and Action Plan (2021 – 2023) lists social prescribing as part of its plan to implement the Health Service Capacity Review and the Healthy Ireland Action Plan (2021 – 2025) commits to launching a Social Prescribing Policy which will see patients referred to non-clinical activities, as a way of positively influencing mental health and wellbeing.
In 2017, the All-Ireland Social Prescribing Network was established with the purpose of championing social prescribing “so that it is valued and understood across the island of Ireland”. The network includes representatives from the health service, academia and the community and voluntary sector on the Island of Ireland. In their All-Ireland Social Prescribing Conference 2022 Report, they note the need for appropriate long term funding and career paths in order to retain highly skilled staff and that referrals could possibly come from sources other than primary care, social housing providers, for example.
They identified numerous challenges to social prescribing in rural areas across Ireland such as limited access to transport links, lack of internet access, the continued stigma relating to accessing supports for mental health and wellbeing, caring commitments amongst others. If communities across the country are to be supported in addressing and meeting health needs, these other factors must be resourced.