Towards Wellbeing For All - Mental and Physical Health
The Programme for Government acknowledged that our “existing measures of economic performance fail to measure matters such as damage to the environment and voluntary work. They also overlook equality of opportunity, distribution of wealth and income and only value public expenditure on the basis of the inputs used, not the outcomes achieved” and committed to introducing a series of indicators that would more accurately measure wellbeing to provide a “holistic view of how our society is faring”.
A ‘Wellbeing Dashboard’ was then developed to provide a snapshot of progress. In developing the Dashboard, the Inter-Departmental Working Group established a list of 35 indicators chosen to be balanced, add value or be of policy relevance, provide for aggregation and dis-aggregation, be readily available and of sufficient quality, and be internationally comparable.
So how are we doing? To gauge public opinion on what matters, and what should therefore be counted as an indicator of Well-being, Social Justice Ireland produced a survey asking people to rank a set of six indicators under each of the Well-being Framework dimensions from one to six, with one being the least important and six being the most important. The six indicators included the indicators used in the Dashboard and datasets readily available from the CSO and other reputable sources. This survey was circulated over the Summer months through our social media channels, our Weekly Digest, and our Members Bulletin. What follows is based on the responses to this survey and our policy proposals under each of the 11 dimensions.
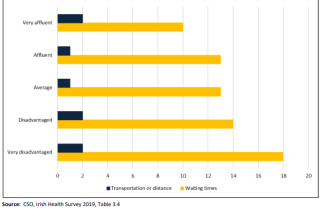
The indicators with the highest weighted ranking under this dimension were Inability to afford adequate healthcare; Outpatient and In-patient Waiting Lists; and Self-reported unmet need for medical attention. The Irish Health Survey 2019 indicates that while two per cent of the population reported an unmet need for health care due to transport or distance, 14 per cent of the population reported an unmet need due to waiting times.[1] The proportion for people who were classified as “very disadvantaged” increases to 18 per cent, almost double that of “very affluent” people (10 per cent) (Chart 1).
Chart 1: % Population with unmet health care needs deprivation quintile and reason, 2019
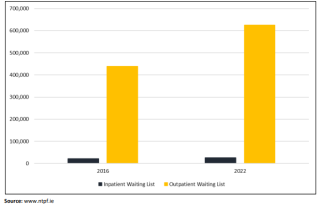
The number of people currently awaiting outpatient treatment in Ireland is 625,679 compared to 568,769 in September 2019, and 438,267 in September 2016. An increase of 43 per cent in outpatient waiting lists over six years. A similar pattern emerges in respect of inpatient waiting lists, with 26,509 people awaiting treatment in September 2022 compared to 22,197 in September 2019 and 17,984 in September 2016, a 47 per cent increase between 2016 and 2022 (Chart 2).
Chart 2: Inpatient and Outpatient Waiting Lists, September 2016 and September 2022
The proportion of people aged 15+ with selfreported unmet need for medical attention is just 2 per cent in 2020 overall, and has remained static since 2018, and is in line with the EU average.
The Child and Adolescent Mental Health Services reported 4,003 children on the waiting list in April 2022 compared to 2,919 in April 2021. 405 of those children had been waiting for more than 12 months.
Policy Priorities
- Ensure that announced budgetary allocations are valid, realistic and transparent and that they take existing commitments into account.
- Complete the roll-out of the Community Health Networks and increase the availability and quality of Primary Care and Social Care services.
- Ensure medical card-coverage for all people who are vulnerable.
- Act effectively to end the current hospital waiting list crisis.
- Create a statutory entitlement to Home Care Services. This will require increased funding, but will save the State money long-term, as home support allows people to remain living in their own homes, rather than entering residential nursing care.
- Implement all aspects of the dementia strategy.
- Adopt a target to reduce the body mass index (BMI) of the population by 5 per cent by 2025.
- Work towards full universal healthcare for all. Ensure new system structures are fit for purpose and publish detailed evidence of how new decisions taken will meet healthcare goals.
- Enhance the process of planning and investment so that the healthcare system can cope with the increase and diversity in population and the ageing of the population projected for the next few decades.
[1] https://www.cso.ie/en/releasesandpublications/ep/p-ihsmr/irishhealthsur…