Budget 2021 must address healthcare inequalities
People should be assured of the required treatment and healthcare in their times of illness and vulnerability. The standard of care available is dependent to a great degree on the resources made available, which in turn are dependent on the expectations of society. Covid-19 put an unprecedented strain on our healthcare system, however the systemic issues and overreliance on acute services which dominated the Irish healthcare infrastructure pre-Covid only served to exacerbate the problem. Spending on the Health Vote to the end of May 2020 stood at €8.3 billion, €1.1 billion above profile and almost exclusively due to current spending in response to the pandemic. While some reductions can be expected over the coming months, ongoing current expenditure should be anticipated with appropriate allocations made. These allocations must be ring-fenced to address ongoing Covid-19 requirements.
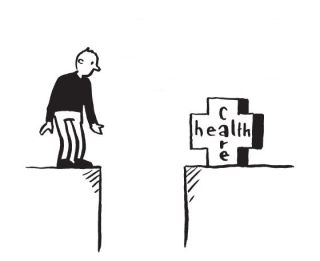
Access to Care
Ireland ranked 21st out of 35 countries in 2016 in a report by Health Consumer Powerhouse published in 2017, but on the issue of accessibility, Ireland ranked among the three worst countries. That report notes that even if the (then) Irish waiting-list target of 18 months were reached, it would still be the worst waiting time situation in Europe. Irish hospitals are working near full capacity. Our complex two-tier system for access to public hospital care means that private patients have speedier access to both diagnostics and treatment, while those in the public system can spend lengthy periods waiting for a first appointment. National Treatment Purchase Fund figures indicate that 86,343 people were waiting for treatment as an in-patient or day case at the end of April 2020, with 5,844 of them waiting for 18 months or longer. Government needs to urgently address these inequalities in the health service and implement a programme that provides access on the basis of need.
Acute Care
Before the pandemic ever reached these shores Irish hospitals were already working near full capacity. The occupancy rate for acute care beds is among the highest in OECD countries, and while having a high utilisation rate of hospital beds can be a sign of hospital efficiency, it can also mean that too many patients are treated at the secondary care level. This is about 20 percentage points higher than the OECD average (which was 75.2 per cent) and the highest in the EU-28. The Covid-19 crisis has seen a policy concentration on acute care, however having appropriate primary care and step-down facilities in place would alleviate the strain on hospitals.
Primary Care
In its report on the Irish healthcare system in 2019 the OECD found it to be hospital-centric, with significant capacity constraints in primary and secondary care and concluded that the current health infrastructure is simply not adequate for current demand and unable to cope with the projected increases due to population ageing—and that was before the pandemic. The new Government needs to ensure that inequalities inherent in our health system are addressed. The implementation of Sláintecare, which received cross-party support in 2016, must be prioritised, with the initial €500m infrastructure allocation provided in the next and five subsequent Budgets. The over-reliance and over-burdening of our acute care system must be reduced by scaling up Community Health Teams and Networks and providing for increased GP coverage, community nursing, public health nursing and community beds.
Mental Health
Mental health is critical to individual well-being, as well as for social and economic participation and yet it is estimated that more than one in six people across EU countries had a mental health issue (in 2016), equivalent to about 84 million people. Young people are especially susceptible to mental health issues and early intervention is key. In 2016 the UN Committee on the Rights of the Child raised concerns about children’s mental health services, including children being admitted to adult psychiatric wards, long waiting lists for access to mental health support, and insufficient out-of-hours services. The report also expressed concern about the high number of suicides among adolescents and stated that Ireland should adopt all-inclusive legislation that addresses the health needs of children. Covid-19 has also had a predictable impact. The College of Psychiatrists of Ireland are currently working on a study based on a survey of 615 consultants, with early indications finding an increase in adverse mental health conditions, suicidal ideation, and self-harm, with specific concerns expressed about younger people with existing mental health issues and older people forced to cocoon. The implementation of the Vision for Change strategy is long overdue. There is an urgent need for effective community services including effective outreach and follow-up programmes for people who have been in-patients in institutions upon their discharge into the wider community. These should provide sheltered housing (high, medium and low supported housing); monitoring of medication; retraining and rehabilitation; and assistance with integration into community.
Persons with a Disability and Carers
People with disabilities were cumulatively affected by a range of decisions made as part of successive austerity Budgets. These included cuts to social welfare payments, changes in medical card eligibility, increased prescription charges, and cuts to supports such as respite, home support hours, and housing adaptation grants. The cumulative effect of changes makes it difficult for some people to continue to live in their communities. Despite Government commissioning work on the issue of a cost of disability payment no steps were taken towards its introduction. If people with a disability are to be equal participants in society, the extra costs generated by disability should not be borne by them alone. The cross-sectional needs of people with disabilities must also be recognised. People with a disability need to be supported, not only by the health service, but through Local Authorities with regard to housing need, through the Department of Social Protection in terms of income supports, as well as by the Department of Education through education and training.