No going back to the two-tiered Health System
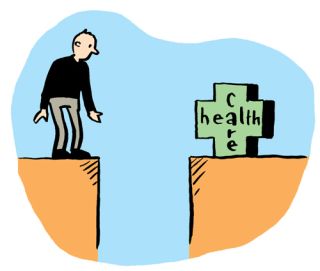
People should be assured of the required treatment and care in their times of illness and vulnerability. The standard of care is dependent to a great degree on the resources made available, which in turn are dependent on the expectations of society.
Covid-19 put an unprecedented strain on our healthcare system, however the systemic issues and overreliance on acute services which dominated the Irish healthcare infrastructure pre-Covid only served to exacerbate the problem.
Access to Care
Ireland ranked 21st out of 35 countries in 2016 in a report by Health Consumer Powerhouse published in 2017, but on the issue of accessibility, Ireland ranked among the three worst countries. That report notes that even if the (then) Irish waiting-list target of 18 months were reached, it would still be the worst waiting time situation in Europe. Irish hospitals are working near full capacity.
According to data from the National Treatment Purchase Fund there were 178,064 people waiting for 18 months or more for outpatient’s treatment in March 2021. This equates to almost three in every 10 of the 628,756 people awaiting treatment that month.
Compared to the same month in previous years, there has been a large increase in the total number of people awaiting treatment for 18 months or more – an increase of 65 per cent on March 2020 and 75 per cent on March 2019. Older people have fared the worst in terms of delays in treatment, with number of older people on outpatient waiting lists for 18 months or more has increased by 68 per cent since 2020 and by 88 per cent since 2019. While still high, the rate of increase among children has not increased to the same extent. Those aged 0-15 years awaiting treatment for 18 months or more increased by 50 per cent on 2020 and 35 per cent on 2019 .
Government needs to urgently address these inequalities in the health service and implement a programme that provides access on the basis of need.
Acute Care
Irish hospitals are working near full capacity. The occupancy rate for acute care beds is among the highest in OECD countries, and while having a high utilisation rate of hospital beds can be a sign of hospital efficiency, it can also mean that too many patients are treated at the secondary care level Primary Care. In 2018, bed occupancy rates for curative (acute) care averaged 73 per cent across EU Member States, but they were 91 per cent in Ireland.
Like the governments of other countries, the Irish government made additional allocations in 2020 to the health sector to deal with the COVID-19 pandemic. These commitments included expanding hospital capacity, developing primary and community-based responses, procurement of medical equipment, and an assistance scheme for private nursing homes. Universal health coverage is a key pre-requisite to improving access to care for vulnerable groups, something, that might be said to be acknowledged in the government’s extension of coverage for GP visits for COVID-19 treatment to the entire population.
The model of healthcare used in Ireland is defined by an over-emphasis on hospitals and acute care rather than primary and social care being more central. However, reform will not happen without prior investment. While recognising the significant additional resources provided in response to the COVID-19 pandemic, it is essential that the resources are deployed in a way which delivers the transformation of the health service in line with Sláintecare.
Proposals: To address the inequalities in our healthcare system and develop a system that is fit for purpose for all, Government needs to:
· Invest the €500m infrastructure allocation set out in Sláintecare.
· Invest €50m in Community Nursing Facilities.
· Invest €150m in the roll-out of community health networks to alleviate pressure on acute services and ensure treatment is provided at the appropriate level of need.
Mental Health
According to the latest available data, the HSE Management Data Report for September 2020, 2,112 children and young people were awaiting supports from the Child and Adolescent Mental Health Service (CAMHS). Of these one in ten were waiting for treatment for 12 months or more. This is a slight proportionate decrease on the same period in 2019 when 11 per cent were waiting in excess of 12 months or more. A mental health crisis is likely to be a prevailing legacy from Covid-19, not just because of the immediate stress; but also the impact of the illness on those who contract it and their wider circle; the impact on healthcare workers and other frontline staff; and the impact on those who live in vulnerable households, including households with domestic abuse .
Proposal: Invest in the full implementation of the Sharing the Vision strategy at an initial cost of €35m and increase funding for programmes dealing with alcoholism and addictions at a cost of €76m.
Read the full text of our Budget Choices 2022 Policy Briefing - Delivering a Fair Recovery - HERE.